
Need Support?
- 719 Arbol, Irving, TX 75039

Need Support?
Maximize collections, eliminate denied claims, and accelerate insurance processing with our specialized DentalXChange solutions and comprehensive billing services.

TransDental specializes in comprehensive billing and revenue cycle management services optimized for dental practices leveraging DentalXChange’s services. Our proven methodologies combine expert DentalXChange platform utilization with strategic billing management to help you collect more revenue, faster, while significantly reducing administrative complexity and operational costs.
Our DentalXChange-certified billing team optimizes your practice revenue through strategic claim management, proactive A/R follow-up, and collection workflows that fully leverage DentalXChange's powerful clearinghouse capabilities.
With first-pass claim acceptance rates consistently exceeding 98%, we minimize costly denials and rejections coding accuracy, comprehensive DentalXChange real-time eligibility verification, and thorough claim scrubbing protocols.
Our certified DentalXChange specialists master every feature of the industry's leading dental clearinghouse platform to optimize electronic claim submission, leverage real-time eligibility verification and utilize advanced ERA processing.
Free your front office staff from complex billing tasks and insurance headaches. We handle all insurance follow-ups, real-time eligibility checks, electronic claim submissions, ERA reconciliation and patient statement generation.
Stay current with constantly evolving insurance requirements, HIPAA security regulations, clearinghouse specifications, and dental billing best practices through our extensively trained billing specialists who receive continuous education.
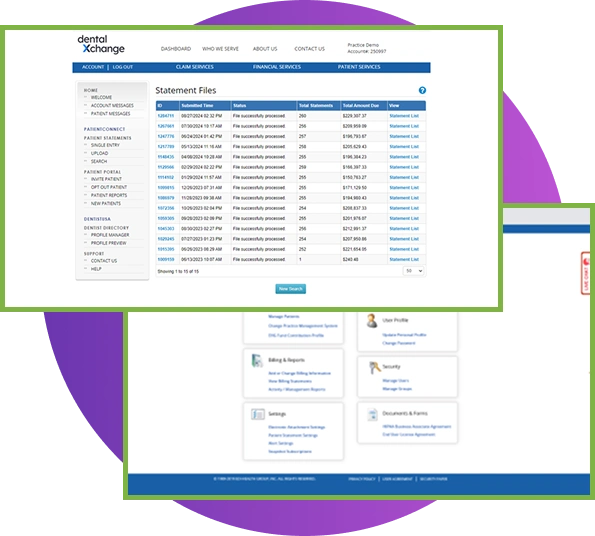
Access comprehensive financial reports and critical KPIs in real-time through integrated reporting that combines your practice management system data with DentalXChange clearinghouse analytics, providing complete transparency.
Complete revenue cycle management solutions leveraging DentalXChange technology for your dental practice.
Pre-appointment benefit verification using DentalXChange's real-time eligibility system confirms coverage status, deductibles, maximums, frequency limitations, and pre-authorization requirements in seconds to eliminate surprise denials.
Electronic claim submission through DentalXChange clearinghouse with multi-stage validation ensures accurate coding, documentation using electronic attachments (NEA), and optimized submission through direct payer connections.
Advanced ERA processing through DentalXChange's comprehensive ERA services automatically posts insurance payments with detailed breakdowns, reducing manual data entry by up to 80% while maintaining perfectly accurate financial records.
Proactive claims tracking using DentalXChange's real-time claims status inquiry services monitors all submitted claims electronically, provides instant adjudication updates, and eliminates time-consuming phone calls to insurance carriers.
Accurate posting of all payments, adjustments, and credits in your practice management system with daily reconciliation leveraging DentalXChange ERA data to ensure financial records remain current and discrepancies resolve immediately.
Proactive follow-up on outstanding claims and patient balances enhanced by DentalXChange clearinghouse intelligence, using real-time claim status data and implementing evidence-based collection strategies that maximize recovery.
Expert denial analysis with strategic appeal preparation leveraging DentalXChange's comprehensive denial reporting identifies root causes using clearinghouse rejection data and submits compelling appeals electronically through DentalXChange.
Expert handling of electronic attachments through DentalXChange's National Electronic Attachment (NEA) infrastructure submits radiographs, clinical documentation, and required attachments electronically, eliminating delays and improving acceptance.
Professional patient statements with flexible payment plans and respectful collection communication improve payment rates through transparent billing informed by real-time eligibility data, convenient online payments, and early intervention strategies.
Detailed monthly reports combining practice management data with DentalXChange clearinghouse analytics covering collections performance, claim submission metrics, eligibility verification accuracy and ERA processing statistics.
Full-service insurance credentialing, CAQH maintenance, & DentalXChange payer enrollment setup handles applications, establishes electronic connections with major payers, monitors deadlines, and ensures active in-network status.
Professional DentalXChange insurance billing gives you more control, not less. Our DentalXChange specialists work directly within your existing system, i.e. your front desk stays focused on patients while we handle complex insurance follow-ups and claim denials behind the scenes.
We analyze your billing processes, workflows, and DentalXChange utilization to identify revenue leakage, denial patterns, and establish baseline performance metrics.
We develop a tailored implementation strategy optimizing DentalXChange feature utilization for maximum efficiency with 24 to 48 hours implementation and minimal disruption.
We provide role-specific training and hands-on DentalXChange platform training with ongoing support and immediate problem resolution ensuring a smooth transition.
Your dedicated account manager conducts regular performance reviews, analyzes DentalXChange clearinghouse reports, and implements refinements.
TransDental offers revenue cycle management services designed for every dental specialty. We help you uncover hidden revenue opportunities, improve billing accuracy, and enhance your practice’s financial performance.
Whatever dental insurance you accept, we’ve got you covered. Transdental’s billing experts navigate every major dental insurance network with 20+ years of payor expertise.























































Schedule your free DentalXChange billing analysis and discover exactly how much revenue is slipping through the cracks in your practice.
TransDental’s DentalXChange optimized billing and RCM services support diverse dental specialties and practice configurations:
General dentistry practices
Pediatric dental offices
Orthodontic practices
Periodontal specialists
Endodontic practices
Oral and maxillofacial surgery centers
Multi-specialty dental groups
Dental service organization (DSO) affiliated practices
Start-up and emerging dental practices
Established practices transitioning to DentalXChange
Most practices are fully operational with our comprehensive services within 24 to 48 hours from initial consultation to complete implementation. We prioritize smooth, professionally managed transitions with minimal disruption to your daily operations, patient care delivery, and staff workflows. If you already have DentalXChange established, implementation is even faster. Expedited implementations can be accommodated for practices with urgent needs, significant billing backlogs, or time-sensitive situations such as staff departures.
Absolutely and without exception. You maintain complete ownership and unrestricted 24/7 access to all your DentalXChange clearinghouse account, practice management system data, patient records, financial information, and system functionality at all times. We work transparently as an extension of your team, and you can access clearinghouse reports, run queries, view claim status, generate statements, post payments, and monitor all financial data and activities whenever you need without any restrictions, delays, or special permissions required.
Your dedicated account manager is available during business hours for consultations, performance reviews, strategic planning sessions, and routine inquiries. Our technical support team provides immediate assistance for time-sensitive matters, urgent billing issues, clearinghouse questions, and system concerns. Most routine inquiries receive resolution within 24 hours or less, urgent matters are addressed immediately with same-day response, and we provide regular proactive communication including monthly performance reports, quarterly business reviews, DentalXChange utilization analytics, and timely alerts about important issues or opportunities.
We offer transparent percentage-based pricing calculated on successfully collected revenue, directly aligning our financial success with yours and ensuring we’re highly motivated to maximize your collections and minimize write-offs. Flat-fee monthly options are also available for practices that prefer predictable costs and simplified budgeting. Hybrid pricing models combining both approaches can be customized. Contact us for a detailed proposal tailored to your practice size, specialty mix, patient volume, insurance mix, and specific service needs and priorities.
Yes, absolutely! This is one of our core specialties. Many practices specifically engage us to resolve substantial accounts receivable backlogs, clean up severely aged claims that have been neglected or improperly worked, recover revenue from denied claims that were never appealed, and address systemic problems that have accumulated over months or years. We specialize in systematic A/R recovery strategies and “clean-up” projects while simultaneously implementing preventive systems, optimized DentalXChange workflows, and comprehensive staff training to eliminate future accumulation and ongoing revenue leakage.
We have extensive experience and established relationships with all major dental insurance carriers through DentalXChange’s comprehensive payer network including Delta Dental (all state plans), MetLife, Cigna, Aetna, Guardian, United Healthcare Dental, Humana Dental, Principal, Ameritas, Mutual of Omaha, Renaissance, GEHA, Anthem, Blue Cross Blue Shield dental plans, and hundreds of regional carriers, employer-specific plans, union plans, and smaller carriers. We also handle Medicaid programs (state-specific), Medicare Part B when applicable for covered dental services, TRICARE/military dental programs, Veterans Affairs dental benefits, and various government assistance and discount programs; all through optimized DentalXChange electronic connectivity.
Our exclusive specialization in dental billing combined with deep DentalXChange clearinghouse expertise sets us fundamentally apart from generalist billing companies. We understand dental-specific billing complexities and nuances, CDT coding requirements and annual updates, dental insurance policy variations and carrier-specific requirements, common denial reasons and effective appeal strategies, and how to fully leverage DentalXChange’s powerful clearinghouse capabilities including real-time eligibility, electronic attachments, ERA processing, claims status tracking, and advanced analytics for maximum financial performance, operational efficiency, and sustained profitability. Our team’s average 15+ years of experience means deep expertise you can trust.
No. If you’re not currently using DentalXChange, we can facilitate setup and enrollment as part of our implementation process. If you already use DentalXChange, we optimize your existing configuration and leverage features you may not be fully utilizing. If you use a different clearinghouse, we can work with your current system, though we’ve found DentalXChange offers superior capabilities for dental-specific claim processing that can significantly improve results.
We’re deeply committed to your satisfaction, success, and practice growth. Your success is literally our business model. If performance doesn’t meet mutually agreed-upon benchmarks, service level agreements, or your expectations, we work immediately and transparently to understand concerns, identify root causes, address any deficiencies, and implement necessary corrections or adjustments. Our flexible agreements allow you to adjust service levels or discontinue services if needed, though our exceptionally high client satisfaction and retention rates reflect our consistent delivery of outstanding results, responsive service, and genuine partnership approach.
Yes, comprehensive training is included as an integral part of our service. We provide thorough initial training during implementation covering roles and responsibilities, DentalXChange platform navigation and features, and we offer ongoing education for your team on topics including their responsibilities within optimized workflows, best practices for clinical documentation and coding, how to communicate effectively with patients about financial matters and payment expectations, how to leverage DentalXChange features effectively, understanding insurance policies and common issues, and staying current with coding updates and regulatory changes. We view staff education as essential to long-term success and optimal collaboration.
Staff turnover is a common challenge in dental practices, and our service model actually helps insulate you from its financial impact. When staff members leave, we provide training for their replacements at no additional cost. Because we maintain the institutional knowledge about your billing processes, insurance relationships, and DentalXChange workflows, there’s continuity even when your team changes. This is one of the key advantages of outsourcing that you don’t lose critical billing expertise when employees leave.
DentalXChange clearinghouse provides significant advantages over direct payer submission including: real-time claim scrubbing that catches errors before submission, instant eligibility verification reducing denials, electronic attachments that eliminate paper delays, ERA auto-posting that saves hours of manual work, real-time claims status tracking without phone calls, comprehensive reporting and analytics, single point of connection to 500+ payers, faster claim processing (typically 24-48 hours vs weeks), and significantly higher first-pass acceptance rates. We help you leverage all these advantages for maximum efficiency and revenue.
Stop leaving money on the table. Let TransDental’s expert billing team handle your revenue cycle management while you focus on providing excellent patient care.
Contact us now to schedule your complimentary practice assessment. We’ll identify opportunities to improve your collections, reduce denials, and streamline your billing operations.
Real Results. Real Practices. Real Success.
Within 2 months of TransDental working in our practice management system, our first-pass acceptance rate jumped from 73% to 96%. They recovered over $47,000 in aging receivables directly through our EHR without disrupting our workflow.
TransDental standardized our billing across three locations and gave me consolidated reporting I never had before. They work seamlessly in our existing EMR with no new software and no learning curve for staff. Our collections are up 28%.
Pediatric insurance is incredibly complex, but TransDental's team handles it all through our practice management system. Their verification process catches coverage issues before appointments, and we've cut denials in half.